Words by Dr Akhanda Upadhaya
“Doctor, I was given a diagnosis of hypertension a year ago, but I refused to take the medication, so this time I came here for a checkup to see if my blood pressure is under control.” A 39-year-old Mrs. K.C. (name altered for privacy) made this comment at a remote Dopla District Hospital. As per her remarks, Mrs. KC is ignorant of the potential risks associated with hypertension and especially high blood pressure. A 35-year-old male, Mr. Dangi (name changed for privacy) also hailing from Dolpa district knows that he has a high blood sugar level. A physician from Nepalgunj had prescribed him a medicine but he ignored taking the medicine. This time, he came to Dolpa District Hospital’s OPD with complaints of blurring of vision and tiredness. Our lab test showed a random blood sugar level 350 mg/dl (HbA1c is not available at our hospital).
“Every day 1-2 people come to OPD for just a Blood pressure checkup, blood sugar level checkup, and cholesterol checkup. They give a history of being diagnosed with such a condition at least 2 years back but they refused to take any prescribed medicine.”
Currently, I have been working at Dolpa District Hospital for 2 years and every day 1-2 people come to OPD for just a blood pressure checkup, blood sugar level checkup, and cholesterol checkup. They give a history of being diagnosed with such a condition at least 2 years back but they refused to take any prescribed medicine. So Mrs. KC and Mr. Dangi are just a representation of the types of patients living with various noncommunicable diseases and always refusing or ignoring to take medicine. Since the last two years I have seen a significant rise in the number of NCDs in Dolpa district, Dolpa district is one of the most remote areas of Nepal. The most common problems I saw here at Dolpa is Hypertension, Chronic obstructive pulmonary disease (COPD), and Diabetes mellitus (DM). Dolpa district is also facing the rising occurrence of non-communicable diseases in recent years. Mental health issues are becoming more and more common. But due to cultural and social issues, patients or their family don’t seek medical help, instead they seek help from traditional healers like Dhami Jhakri. Due to use of tobacco, alcohol and unsafe sexual behavior, the school-aged youth are facing significant mental health issues.
“The most common problems I saw here at Dolpa is Hypertension, Chronic obstructive pulmonary disease (COPD), and Diabetes mellitus (DM). Dolpa district is also facing the rising occurrence of non-communicable diseases in recent years. Mental health issues are becoming more and more common.”
Government Initiative
According to the Ministry of Health and Population of the Nepalese government, NCDs are a significant public health issue in Nepal, contributing to almost 60% of all yearly fatalities in 2014 (WHO). Additionally, the Government of Nepal launched the Package of Essential Non-Contagious Diseases (PEN) in every state of the country, which aims to screen, treat, and promptly refer people who have been identified as having cardiovascular disease, COPD, cancer, diabetes mellitus, or mental health issues by Health Posts to District Hospitals. Sadly, the local government is unaware of this and spends the majority of the budget without a clear strategy, despite the fact that the government provides significant funding for basic equipment and drug purchases as well as for training healthcare professionals. There are 8 palikas in Dolpa, but they have never implemented the program for screening NCDs, and they even lack basic supplies of medication for individuals who have been diagnosed with NCDs.
Local Government Initiative in Dolpa
Every palika has its own health office (Swasthya sakha) that is responsible for overseeing the distribution of medication to the palikas’ population. The office and its coordinator work in conjunction with the District health service office. However, only one Palika is aware of NCD at this time. Every palika health employee receives PEN training from the health service office. Even after returning from the training, they do not perform a straightforward NCD screening test on those who attend a health facility. Additionally, the Nepali government and state governments now provide palika enough money to purchase tools and test kits including a blood pressure cuff, a glucometer, and a weighing scale. Additionally, they do not implement any programs to educate their particular palikas on NCD prevention. I never heard the local palikas create an awareness effort during these two years. Because the most frequent modifiable risk factors for NCD are behaviors like tobacco use, hazardous alcohol use, consumption of a high percentage of unhealthy foods, such as a diet rich in salt and low in fruits and vegetables, and physical inactivity. If we regularly educate the public about it and its effects, we may be able to avoid NCD in rural populations. Like in the upper and lower dolpas, the majority of people drink Tibetan tea, which is prepared with a lot of ghee and salt. Even at our hospital’s OPD, those who drink a lot of tea from Tibet often have high blood pressure and high cholesterol levels.
“In places with limited resources, mid-level health workers may carry out such interventions, but owing to the absence of ongoing oversight, local level health workers only get training from district health service offices and do not put that training into practice in accordance with government guidelines for Nepal.”
Immediate need of Action to prevent NCD in rural area
In order to meet the demands of NCDs, the government of Nepal now implements PEN interventions in low resource settings. In places with limited resources, mid-level health workers may carry out such interventions, but owing to the absence of ongoing oversight, local level health workers only get training from district health service offices and do not put that training into practice in accordance with government guidelines for Nepal. Particularly in Dolpa, people with NCDs frequently experience extreme suffering because those who have high blood pressure but are not taking medication or getting regular checkups arrive at the district hospital with a stroke and because of poor road access, transportation, and medical facilities, they often do not receive adequate care on time. In cases when we referred them, however, their financial situation prevented them from traveling outside of the district, so a family member took them to Dhami jhakri. In order to manage the growing burden of NCDs in rural areas, there is an urgent need for infrastructure, a solid referral system, and frequent monitoring of NCDs at the local level. The frequent monitoring at the local level is also necessary to determine whether or not they are using their budget appropriately.
Condition at Dolpa District Hospital
Dolpa, in Karnali province, is one of Nepal’s most isolated regions. Despite limited resources, we are providing free basic and emergency medical services. We have not yet concentrated on community NCD diagnosis, but we have spread information on NCDs through our hospital’s Facebook page. Every day at our hospital, 3–4 patients come with high blood pressure; we maintained track of them, but after their first visit, they stopped coming for follow-up owing to the poor road access. As a result, we now keep an NCD registry where we save patient contact information. If a patient’s contact information is lost or unavailable, we ask the appropriate health post person to coordinate with them. Our biggest issue is that we have a lot of trouble handling NCD patients since there aren’t enough qualified staff members and structured referrals.
Conclusion
In the remote landscapes of Dolpa, where echoes of traditional healing methods resonate more than modern medical interventions, the battle against noncommunicable diseases (NCDs) is both silent and urgent. Patients like Mrs. K.C. and Mr. Dangi are just examples of a larger challenge: individuals aware of their health conditions yet reluctant to embrace medical solutions. As NCDs surge in Dolpa, marked by hypertension, COPD, and diabetes, a glaring disparity emerges between government initiatives and ground-level implementation. The Package of Essential Non-Contagious Diseases (PEN) remains a largely unexplored resource, with local governments unaware or unmotivated to address the growing NCD burden. The absence of awareness programs and the prevalence of modifiable risk factors like dietary habits exacerbate the situation. Urgent action is imperative, calling for infrastructure development, robust referral systems, and consistent local-level monitoring. Dolpa District Hospital stands as a beacon of hope, yet its struggle lies in insufficient staffing and structured referrals. The narrative unfolding in Dolpa beckons not just for medical intervention but a systemic transformation to combat NCDs in the heart of rural Nepal.
About The Author
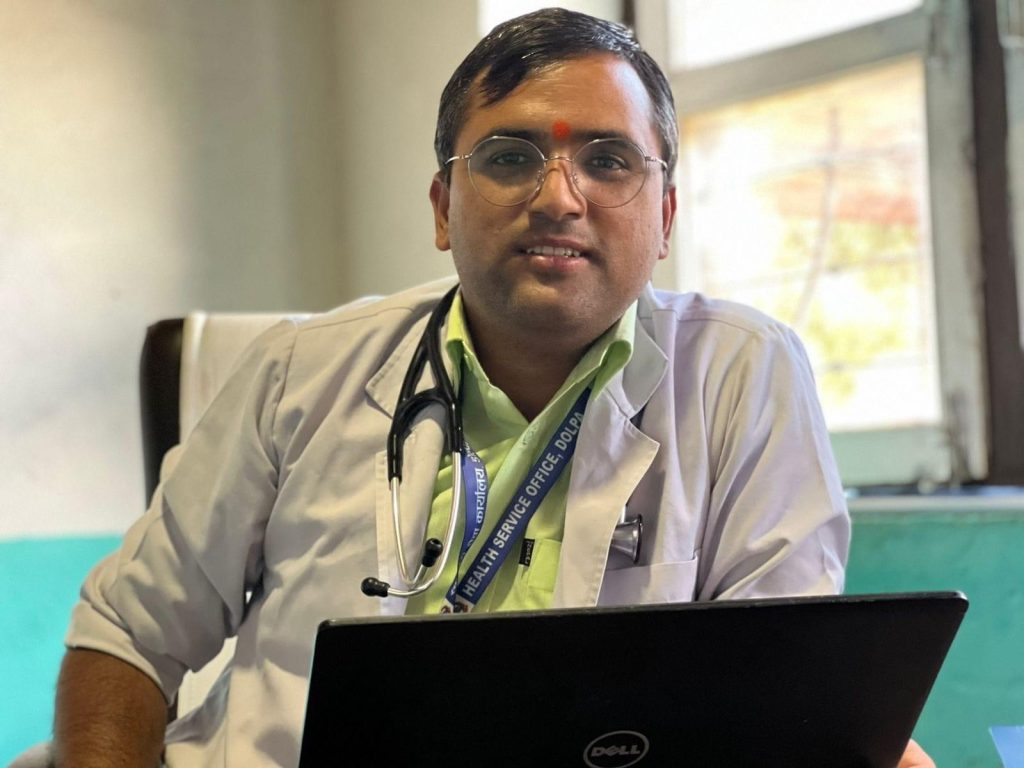
By encouraging local deliveries at Dolpa Hospital, he hoped to reduce the need for them to travel to Surkhet or Nepalgunj for childbirth. Recognizing the financial challenges faced by the community, Dr. Upadhaya and his team along with support from Himalayan Family Healthcare Project, USA, established the “Poor People Fund” which has enabled them to offer essential medical services free of charge. His current focus emphasizes his commitment to preventative healthcare by increasing knowledge of vector-borne infections and Non-Communicable infections (NCDs) in Nepal’s rural areas
 Medicosnext
Medicosnext




