summary:
A 27 year old unmarried, sexually active, obese woman with irregular menstrual cycle presented with symptoms of acute intermittent lower abdominal cramps for one day. On examination, general condition was fair and vitals were stable. On abdominal examination, it was soft and tender in right iliac fossa. P/S examination revealed healthy cervix with minimal discharge. On per vaginal examination, uterus could not be assessed and bilateral fornices were full. Ultrasonographyof abdomen and pelvis showed a left ovarian cyst of 12×11 cm with mixed echogenicity, a right ovarian cyst of 11×9 cm, and right nephrolithiasis. Uterus was anteverted, normal in size, and no free fluid was seen. Bilateral laparoscopic cystectomy was performed and a significant amount of normal ovarian tissue was left behind. Cut-section of the gross specimen showed hair, sebaceous fluid, and cheesy material. Histopathology showed bilateral mature teratoma of ovary (dermoid ovarian cyst).
Introduction
Dermoid cyst or mature teratoma of ovary is the most common benign tumor of ovary in young and middle-aged woman1. Bilateral dermoid cyst in young woman is a difficult condition to manage, because a considerable amount of ovarian tissue needs to be preserved for future fertility. There are relatively less cases of bilateral dermoid ovarian cyst in young women.
Case presentation
History: A 27 year old sexually active, unmarried, obese woman presented with acute lower abdominal pain for one day. There was history of irregular menstrual cycle and last period was one month back. There was no bowel or bladder disturbance, no history of weight loss or decreased appetite. There was no significant past medical and surgical history. Family history was not significant.

General physical examination
General condition: Fair. Obese. No jaundice, pallor, lymphadenopathy, or edema. Vitals were stable. Breast and thyroid examinations were normal. Per abdominal examination: Abdominal obesity present with tenderness in right iliac fossa. No mass was appreciated and there was no ascites. P/S examination revealed healthy cervix with minimal discharge. P/V examination: uterus could not be assessed and bilateral fornices fullness was noticed.
Investigations: All the routine investigations were within normal limits. Renal function test, liver function test, and chest x-ray were normal. Ultrasonography of abdomen and pelvis showed a left ovarian cyst of 12×11 cm with mixed echogenicity, a right ovarian cyst of 11×9 cm, and right nephrolithiasis. Uterus was anteverted, normal in size, and no free fluid was seen. Urology consultation for nephrolithiasis was done and no active intervention was advised with a plan to follow up.
Treatment: Bilateral laparoscopic cystectomy was done under general anesthesia.
Intraoperative findings: Left-sided twisted dermoid cyst of 12×10 cm, right sided dermoid cyst of 12×8 cm with another small simple cyst. Capsules were intact bilaterally, without adhesions; no free fluid. Bilateral tubes seemed normal. Uterus was anteverted and normal in size. Cut- section: Dermoid cyst contained hair, sebaceous fluid, and cheesy material.
Outcome: Postoperative stay of the patient was uneventful. Patient was discharged on the fourth postoperative day. Histopathology of cystic wall tissue confirmed the diagnosis of bilateral mature teratoma of ovary.
Discussion
Dermoid cyst constitutes 10–25% of all the neoplasms of ovary. Peak incidence is observed in the age group of 25–45 years1,2. It is usually a benign germ cell tumor that is rarely malignant3. Bilateral dermoid cyst of ovaries may be seen in 10% of cases. Dermoid cyst is usually unilocular, containing hair and sebaceous material, with squamous epithelial lining. In some cases, bone, teeth, thyroid tissue, cartilage, and bronchial mucous membrane may also be found. It may be associated with mucinous cystadenoma in up to 40% of cases4. Within the inner surface of dermoid cyst, there is area of solid projection known as Rokitansky’s protuberance, and it is covered by skin, sebaceous glands, and sometimes by teeth and bones. There are theories which suggest that dermoid cyst develops from genetic material from a single oocyte. The oocytes which are capable of parthenogenesis result from an arrest of development of oocyte after meosis I. So, almost all mature cystic teratomas have a karyotype of 46, XX5.
Complicatons: Dermoids may undergo torsion in up to 15% of cases because of long pedicle and heavy weight, and it was observed in our case6. Spontaneous rupture is rare due to its thick wall. In case of rupture, it may lead to chemical or granulomatous peritonitis. Risk of recurrence is 3–4%, and it rarely becomes malignant (1.7%, squamous cell carcinoma)7.
 Diagnosis: Ultrasonography shows “tip of the iceberg” sign, which is due to acoustic shadowing caused by calcifications or fat. There may be hair-fluid or fat-fluid levels with clear demarcation. Presence of hair is frequently found in mature cystic teratoma8. Rokitansky’s protuberance is characteristic of dermoid cyst.
Diagnosis: Ultrasonography shows “tip of the iceberg” sign, which is due to acoustic shadowing caused by calcifications or fat. There may be hair-fluid or fat-fluid levels with clear demarcation. Presence of hair is frequently found in mature cystic teratoma8. Rokitansky’s protuberance is characteristic of dermoid cyst.
Treatment: Most surgeries for benign ovarian disease can be done 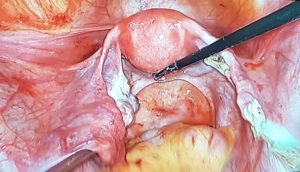 laparoscopically. Shorter recovery time, duration of hospital stay, and lesser chance of adhesion formation are major advantages of laparoscopic surgery compared to laparatomy9, 10. Randomized clinical trials also show less burden of febrile morbidity and a lesser chance of urinary tract infection, postoperative complications, including postoperative pain with laparoscopic cystectomy11. A known disadvantage of laparoscopic cystectomy is the risk of spillage cyst content or cells into the peritonium12,13. This may cause peritonitis or spread malignancy if the tumor is malignant. Hence, laparoscopic surgery should be reserved for those patients in whom the chance of malignancy is very low.
laparoscopically. Shorter recovery time, duration of hospital stay, and lesser chance of adhesion formation are major advantages of laparoscopic surgery compared to laparatomy9, 10. Randomized clinical trials also show less burden of febrile morbidity and a lesser chance of urinary tract infection, postoperative complications, including postoperative pain with laparoscopic cystectomy11. A known disadvantage of laparoscopic cystectomy is the risk of spillage cyst content or cells into the peritonium12,13. This may cause peritonitis or spread malignancy if the tumor is malignant. Hence, laparoscopic surgery should be reserved for those patients in whom the chance of malignancy is very low.
To summarize, laparoscopic cystectomy is the preferred technique for dermoid cyst, because it is associated with a smaller scar, lesser duration of hospital stay, and lower frequency of postoperative complications like adhesion formation pain, compared to laparotomy. Conditions in which the open method are when the surgeon is not experienced in using laparoscope, when there are dense adhesions, very large cyst, or when there is a risk of malignancy.
References:
- Prat J. Female Reproductive System. In: Damjanov I, Linder J, Anderson WAD, editors. Anderson’s pathology. 10th ed. St Louis, Mo: Mosby; 1996. pp. 2231–2309
- Talerman A. Germ cell tumours of the ovary. In: Blaustein’s Pathology of the Female Genital Tract, Kurman RJ (Ed), Springer Verlag, New York 1994. p.849.
- Berek JS. Epithelial ovarian cancer. In: Practical Gynecologic Oncology, 4th, Berek JS, Hacker NF (Eds), Lippincott Williams & Wilkins, Philadelphia 2005. p.443.
- Ueda G, Fujita M, Ogawa H, Sawada M, Inoue M, Tanizawa O. Adenocarcinoma in a benign cystic teratoma of the ovary: report of a case with a long survival period. GynecolOncol. 1993 Feb; 48(2):259-63
- Caspi B, Lerner-Geva L, Dahan M, Chetrit A, Modan B, Hagay Z, Appelman Z. A possible genetic factor in the pathogenesis of ovarian dermoidcysts.GynecolObstet Invest. 2003;56(4):203-6. Epub 2003 Nov 11.
- Ahmed M.Abbas,EsraaGamal, EsraaTalaat,AmeraM.Sheha. Torsion of huge dermoid cyst in adolescent girl: A case report. Middle East Fertility Society JournalVolume 22, Issue 3, September 2017, Pages 236-239
- Ayhan A, Bukulmez O, Genc C, et al. Mature cystic teratomas of the ovary: case series from one institution over 34 years. Eur J ObstetGynecolReprodBiol 2000; 88:153.
- Patel MD, Feldstein VA, Lipson SD, et al. Cystic teratomas of the ovary: diagnostic value of sonography. AJR Am J Roentgenol 1998; 171:1061.
- Hidlebaugh DA, Vulgaropulos S, Orr RK. Treating adnexal masses. Operative laparoscopy vs. laparotomy. J Reprod Med 1997; 42:551.
- Bisharah M, Tulandi T. Laparoscopic preservation of ovarian function: an underused procedure. Am J ObstetGynecol 2003; 188:367.
- Medeiros LR, Fachel JM, Garry R, et al. Laparoscopy versus laparotomy for benign ovarian tumours. Cochrane Database Syst Rev 2005; :CD004751.
- Canis M, Rabischong B, Botchorishvili R, et al. Risk of spread of ovarian cancer after laparoscopic surgery. CurrOpinObstetGynecol 2001; 13:9.
- Leminen A, Lehtovirta P. Spread of ovarian cancer after laparoscopic surgery: report of eight cases. GynecolOncol 1999; 75:387.
 Medicosnext
Medicosnext




