Minimally invasive image guided procedures are in a budding stage in our country, and only a few, if none, cases have been done till date. These facilities are now available in our hospital. Patients of brain stroke, brain aneurysm, and brain vascular malformation can be managed by these methods (without opening skull) for better outcome and less complications.
Various other interventional procedures are also carried out in the hospital by the interventional radiology team. In a span of nine months or so, this team has performed procedures like mechanical thrombectomy for stroke, cerebral aneurysms coiling (both ruptured and unruptured), cerebral AVM, cerebral AVF, renal AML embolization, left gastric artery pseudoaneurysm embolization in a patient with upper GI bleeding, and subclavian venoplasty for severe venous stenosis in a CKD patient with brachio-cephalic fistula for dialysis.
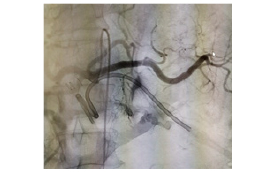
1. Opening of occluded brain vesselby putting small pipe from leg vessel
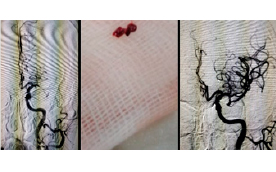
2. Opening of occluded brain vessel by putting small pipe from leg vessel


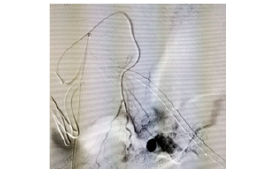
9. Left gastric vein pseudoaneurysm in pt with UGI bleed- embolization
What is stroke/Is treatment of stroke possible in Nepal ? YES!
Stroke can be defined as a loss of brain function due to the disturbance in the blood supply to the brain. Since stroke can cause significant morbidity due to permanent neurological damage, or even death, it is classified as a medical emergency. Hence, it is of utmost importance that stroke symptoms are recognized early and treated to minimize any adverse effects. One of the popular systems for prompt recognition of stroke, FAST (facial drooping, arm weakness, speech difficulties, and time), helps by identifying the stroke by means of recognizing various symptoms. Since time is of the essence during a stroke, the patient must be immediately referred to a hospital for medical care.
Rapid restoration of the cerebral blood flow helps to save as many brain cells as possible, resulting in less number of cell deaths and eventually decreasing the extent and degree of morbidity. Therefore, neurological examination (like NIHSS) is followed by imaging (CT or MRI and arteriography) with an intent to diagnose the case of stroke, know the extent of damage and the salvageable tissue, and initiate the appropriate therapeutic procedure as soon as possible. The treatment itself has undergone major modifications over the century. Stroke treatment protocol is time-dependent and depends upon the following: time of presentation of the patient to the medical center and facilities available at the said center.
As per the latest AHA guidelines, the treatment of choice within four-and-a-half hour of the symptom onset is intravenous thrombolysis (rTPA), which involves using pharmacological means for breaking down the blood clots. Beyond this window period for intravenous thrombolysis, definitive therapy is aimed at removing blockage by using mechanical instruments for removal of the clot (thrombectomy).
Mechanical thrombectomy is the treatment of choice within six hours of the onset of symptoms for anterior circulation stroke, and 24 hours for posterior circulation stroke. However, with latest trials, emphasis has been given for the perfusion mismatch and penumbra to core ratio and the mechanical thrombectomy can be carried out up to 24 hours in favorable conditions. These devices can be used in the larger arteries, where the caliber of the cerebral vessel is 2-5 mm, utilizing catheters to deliver a clot-disrupting or retrieval device to the occluding thromboembolus that is occluding a cerebral artery. Removal of clot by such mechanical thrombectomy devices, in contrast to pharmacological thrombolytics, can be done in a matter of minutes, thus increasing the speed of recanalization and decreasing the chance of more tissue ischemia/infarct, and also reducing the chance of reperfusion injury. Since the recanalization can be done in a very short period of time, mechanical thrombectomy provides a longer time window for use, as compared to thrombolytics.
Mechanical recanalization techniques can be classified by two major approaches—proximal and distal thrombectomy. In proximal thrombectomy, the microcatheter is placed in proximity to the site of occlusion and manual suction thrombectomy is performed by advancing an aspiration catheter at the proximal surface of the thrombus, which is retrieved once manual aspiration is applied under constant negative pressure.
On the other hand, in distal thrombectomy, the occlusion site is crossed over by using a microcatheter. Stent retrievers, which are stent-like thrombectomy devices, are used to remove the clot. This device helps in immediate flow restoration to the distal segments by deployment of the stent even before the clot is removed, thus even faster tissue reperfusion, followed by the clot removal. At the end of the procedure, the stent is removed, thereby avoiding the complications of permanent stent implantation, such as increased haemorrhagic risks giving rise to due need for double anti-platelet medication and the risk of in-stent thrombosis or stenosis.
To summarize, mechanical thrombectomy may be employed either as a standalone treatment or as an adjunct to IV tPA and has several potential advantages, including a wider time window (up to six hours), the capacity for use in coagulopathic patients, and higher recanalization rates, which is unprecedented, with additional benefit of lower haemorrhagic complications. Therefore, it can be concluded that mechanical recanalization technique in the treatment of acute ischemic stroke has undoubtedly broadened the spectrum of patients for treatment.
 Medicosnext
Medicosnext




