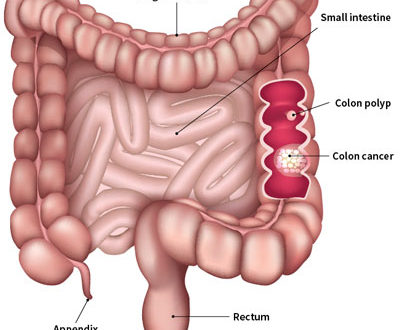
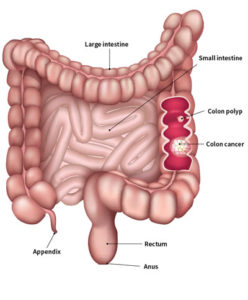
 Colorectal cancer is cancer that affects the large intestine and the rectum. Colon cancer and rectal cancer are often grouped together, because they are related diseases with many of the same characteristics.The most common type is adenocarcinoma. Colorectal cancer is the third most common cancer in the world (after lung and breast), and the second most common cause of cancer death worldwide. When males and females are considered separately, it is the third most common cancer in males and the second most common cancer in females. In 2018, there were about 1.8 million new colorectal cancer cases and 900,000 deaths from this disease worldwide. Reliable statistics are lacking in Nepal, but colorectal cancer is definitely increasing in incidence in our part of the world as well. Of particular concern is the significant increase in aggressive colorectal cancers in young adults in recent years.
Colorectal cancer is cancer that affects the large intestine and the rectum. Colon cancer and rectal cancer are often grouped together, because they are related diseases with many of the same characteristics.The most common type is adenocarcinoma. Colorectal cancer is the third most common cancer in the world (after lung and breast), and the second most common cause of cancer death worldwide. When males and females are considered separately, it is the third most common cancer in males and the second most common cancer in females. In 2018, there were about 1.8 million new colorectal cancer cases and 900,000 deaths from this disease worldwide. Reliable statistics are lacking in Nepal, but colorectal cancer is definitely increasing in incidence in our part of the world as well. Of particular concern is the significant increase in aggressive colorectal cancers in young adults in recent years.
Colorectal cancer usually starts as a small polyp that is initially benign. Polyps are abnormal tissue growths in the lining of the colon and rectum. There are various types of polyps, for example, hyperplastic or inflammatory polyps usually do not progress to cancer, whereas adenomatous polyps can progress to colorectal cancer over time. The process by which a precancerous polyp gradually grows in size, accumulates additional mutations, then eventually transforms into a malignant growth, takes several years.
Once a polyp becomes cancerous, it tends to grow deeper within the wall of the intestine, and as the disease progresses further, cancer cells spread to lymph nodes as well as through the bloodstream to other parts of the body.
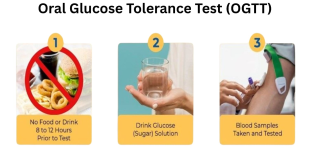
The risk of developing colorectal cancer increases with age; more than 90% of these cases occur in people over the age of 45 years. Other risk factors include a high dietary intake of red meats and animal fats; a low intake of fiber, fruits, and vegetables; a sedentary lifestyle; obesity; smoking; excessive alcohol use; and type 2 diabetes mellitus. Patients with inflammatory bowel disease—ulcerative colitis and Crohn’s disease—are at increased risk of colorectal cancer, as are people with a personal or family history of colorectal polyps and cancer. Certain families have hereditary cancer syndromes, such as familial adenomatous polyposis and Lynch syndrome, which confer a high risk of colorectal cancer at a young age.
Most patients with colorectal cancer are asymptomatic, particularly early in the course of the disease. Some patients may notice bleeding in stools, bowel habit changes (with diarrhea, constipation, or change in stool size), while others may have abdominal pain, bloating, and weight loss. Sometimes, colorectal tumors are detected in patients undergoing work-up of anemia.
Since colorectal cancer has few symptoms, regular screening is recommended. Screening—as opposed to diagnostic testing—involves performing a test to detect the disease in the absence of any symptoms. Current guidelines recommend screening for all individuals, starting at the age of 45 years. Screening is started earlier in people who are at higher risk of colorectal polyps and cancer (such as those with inflammatory bowel disease or a family history of colorectal cancer). Screening is beneficial for two main reasons: colorectal cancer is preventable if polyps that lead to the cancer are detected and removed, and it is curable if the cancer is detected in its early stages.
Colonoscopy, during which the entire colon is visually examined, is currently the gold standard screening test. Polyps can be identified, and in many cases removed, at the time of colonoscopy. Biopsies of any larger masses can be taken as well. A colonoscopy is also the most commonly performed diagnostic test to evaluate the large intestine in patients who present with any of the symptoms listed earlier. Other screening methods include fecal occult blood testing and fecal immuno testing, flexible sigmoidoscopy (during which the rectum and lower portion of the colon are visually examined), and double contrast barium enema. In recent years, newer modalities, including stool DNA testing and virtual colonoscopy (CT scan colonography), have also been used for colorectal cancer screening.
Once colorectal cancer is diagnosed, patients undergo staging to check for metastatic disease, usually with CT scans of the chest, abdomen, and pelvis. Patients with rectal cancer will also have an MRI of the pelvis or an endorectal ultrasound for locoregional staging. Routine blood tests and a serum carcinoembryonic antigen (CEA) level are also checked.
Treatment of colorectal cancer is tailored as per the stage of the disease. Patients with non-metastatic colon cancer undergo surgery for resection of the concerned part of the colon, along with the mesocolon and the lymph nodes contained therein. After final pathologic staging, patients with locally advanced disease are considered for adjuvant chemotherapy.
The treatment of rectal cancer involves a more complex algorithm. Early rectal cancer is usually treated by radical surgery, using the principles of total mesorectal excision. Selected patients with very early rectal cancer with favorable features can be treated with transanal full-thickness wide local excision of the tumor. Locally advanced rectal cancer patients receive preoperative (neoadjuvant) radiation therapy, with or without concurrent chemotherapy. This is followed by radical surgery, then completion chemotherapy. Clinical trials are currently ongoing to determine the role and optimal regimen of neoadjuvant chemotherapy in locally advanced rectal cancer.
Metastatic colorectal cancer is usually treated with palliative chemotherapy. Palliative radiation can also have a role. Selected patients with oligo-metastatic disease (limited spread) can still be treated with curative intent – with a combination of systemic chemotherapy and radical surgery, as well as radiation therapy in certain patients.
Surgery for colorectal cancer can be done with open as well as minimally invasive (laparoscopic or robotic) approaches, with equivalent oncologic outcomes. The benefits of laparoscopic surgery include smaller incisions, better cosmesis, decreased pain, decreased blood loss, decrease in hospital stay, and faster recovery. It is also important to have specialized surgical treatment; studies have shown that patients treated by colorectal surgeons (experts in the surgical and non-surgical treatment of benign and malignant diseases of the colon, rectum, and anus) are more likely to survive colorectal cancer.
Colorectal cancer has an excellent prognosis when diagnosed and treated early. Five-year survival for localized (early) disease is 90 percent. Patients with spread to surrounding tissues or organs, and/or the regional lymph nodes (locally advanced disease), have a five-year survival rate of 71 percent. However, in patients with spread to distant parts of the body (metastatic disease), the five-year survival rate drops to 14 percent. This once again emphasizes the importance of screening in order to catch these cancers early, which in turn, translates to better outcomes for patients.
March is colorectal cancer awareness month, and it is important to use the opportunity to increase knowledge and awareness about this disease amongst the public (and indeed, within the medical fraternity). Information about risk factors, screening, and treatment options can help dispel myths and help patients and families. Patients and doctors alike need to be cognizant of the fact that colorectal cancer may have very vague symptoms, and that most patients may not have any symptoms at all. The disparity in survival rates between patients with early, as compared to advanced, disease, illustrates how screening and early detection can save lives. Particularly, any patients with unexplained bleeding in stools or bowel habit changes—even in young adults—should not be taken lightly, and should undergo a thorough and adequate work-up to rule out underlying malignancy.
Colorectal cancer is preventable, treatable, and beatable. We as a society need to come together and raise awareness about this disease for everyone’s benefit.
 Medicosnext
Medicosnext