Words By Dr. Bodhraj Acharya
vWD manifests in three primary types: Type 1, Type 2, and Type 3. Delving deeper, Type 2 subdivides further into 2A, 2B, 2M, and 2N. These subcategories mirror the disease’s myriad clinical presentations and the varying underlying molecular defects.
In many nations, the true prevalence of Von Willebrand Disease remains concealed, largely overshadowed by the paucity of advanced medical infrastructure and diagnostic tools.
Von Willebrand Disease (vWD) stands as an enigma in the world of genetic disorders. The disease is named after the Finnish physician Erik von Willebrand who unveiled its existence back in 1926. After almost a century of discovery, VWD’s mysteries still remain far from fully understood. It remains the most prevalent inherited bleeding disorder worldwide, affecting approximately 1 in 1,000 people irrespective of gender. This contrasts with hemophilia, which predominantly affects males, remember the disease caused a great deal of suffering and tragedy in the royal families of Europe. The Spanish royal family also lost several children to hemophilia.

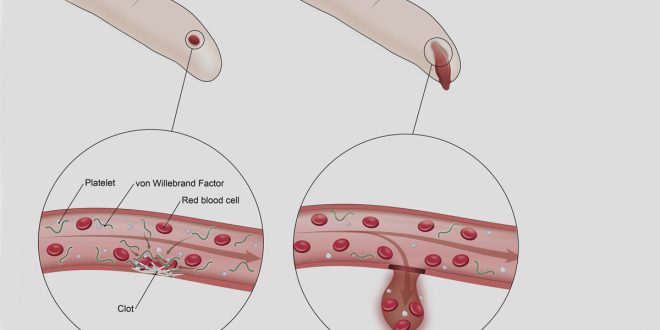
Getting back to Von Willebrand Disease, VWD is marked by a deficiency or dysfunction in the Von Willebrand factor (VWF), a paramount blood-clotting protein. VWF is not just any ordinary protein; it plays a dual role in hemostasis. Firstly, it acts as an anchor, holding platelets in place at the site of a vascular injury. Secondly, it stabilizes factor VIII, another indispensable clotting protein. The repercussions of its absence or malfunction are severe, ranging from prolonged bleeding and susceptibility to bruising to extreme cases that can result in life-threatening hemorrhages.
The true intrigue of this disease lies in its sheer variability. vWD manifests in three primary types: Type 1, Type 2, and Type 3. Delving deeper, Type 2 subdivides further into 2A, 2B, 2M, and 2N. These subcategories mirror the disease’s myriad clinical presentations and the varying underlying molecular defects. This vast heterogeneity renders diagnosis and treatment quite intricate. The silver lining is that with the progress of medical science, our grasp of the labyrinth of VWD’s pathophysiology strengthens.
Diagnosis of vWD
Diagnosing VWD is a comprehensive process that demands a blend of clinical acumen and precise laboratory testing. The initial step usually entails a meticulous clinical evaluation, where a patient’s history is scrutinized for previous bleeding episodes, any relevant family medical history, and potential medication influences.
The standard laboratory toolkit for VWD includes tests such as measuring plasma levels of VWF antigen (VWF:Ag) to gauge the protein quantity, VWF ristocetin cofactor activity (VWF:RCo) to evaluate its functionality, and factor VIII coagulant activity (FVIII:C) to discern the clotting potential. Some situations call for specialized tests like multimer analysis, particularly when suspecting specific subtypes. However, interpreting these results is where the real challenge lies. Borderline cases or those influenced by external factors like inflammation (which can elevate VWF levels) further complicate diagnosis. Consequently, retests are often warranted alongside additional assays. In our modern age, genetic testing also emerges as an indispensable tool, not only cementing diagnoses but also streamlining the classification of VWD subtypes.
Interesting Facts:
- Historical Context: The first recognized case of VWD was in a 5-year-old girl from the Åland Islands in 1924. She suffered from severe bleeding episodes, which prompted Dr. Erik von Willebrand to study her case and subsequently identify the disease.
- Pregnancy and vWD: Women with vWD can experience increased bleeding during their menstrual cycles and may have challenges during childbirth. However, it’s fascinating that VWF levels often increase naturally during pregnancy, which can, at times, alleviate some bleeding concerns.
- Treatment Evolution: Treatment have significantly evolved over time. Initially, patients were treated with fresh frozen plasma. Today, they have access to desmopressin (a synthetic hormone) and VWF concentrates.
- Animal Occurrence: VWD isn’t exclusive to humans. Dogs, particularly certain breeds like Doberman Pinschers, are known to inherit it.
Von Willebrand Disease is not merely a singular, straightforward ailment. It is an intricate puzzle demanding a multidisciplinary approach for optimal diagnosis and management. As we unearth more of its intricacies, we inch closer to comprehending not just VWD but the vast, delicate ballet of hemostasis and clotting disorders.
In many nations, the true prevalence of Von Willebrand Disease remains concealed, largely overshadowed by the paucity of advanced medical infrastructure and diagnostic tools. Many individuals suffer in silence, unaware of the underlying cause of their bleeding episodes. The lack of readily available laboratory tests further exacerbates this situation, making it challenging to ascertain an accurate diagnosis. Early intervention and timely management are pivotal in ensuring a quality life for those afflicted. Without these diagnostic capabilities, countless individuals remain at risk, underscoring the pressing need for global healthcare equality and the widespread availability of diagnostic tools. This not only underscores the urgency of bridging the healthcare disparity gap but also highlights the importance of raising awareness, even as science continues to unravel the intricacies of this enigmatic disease.
 Medicosnext
Medicosnext