
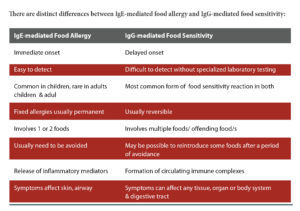
Many people exhibit chronic food sensitivity reactions to specific food antigens. Unlike the immediate effects of IgE-mediated allergy, IgG-mediated food sensitivity reactions may take several hours or days to appear. Controlled removal of the problem foods from the diet will, in many cases, lead to rapid improvement in the patient’s condition.
Type 1 (Immediate Onset)
IgE-mediated Food Allergy
IgE-mediated food reactions are immediate in onset, and usually involve symptoms such as abdominal cramping, diarrhea, skin rashes, hives, swelling, wheezing, or the most extreme reaction, anaphylaxis. When provoked by a recognized food antigen, IgE antibodies promote mast cell degranulation and the release of histamine and other inflammatory mediators.
Type 3 (Delayed Onset)
IgG-mediated Food Sensitivity
IgG-mediated food reactions (also referred to as food sensitivity, food intolerance) are more subtle in their presentation, often occurring hours to days after exposure to food antigens. Unlike IgE-mediated food reactions, IgG-mediated food reactions produce symptoms that are cumulative in nature. Instead of attaching to mast cells, like the IgE antibodies, IgG antibodies bind directly to food as it enters the bloodstream, forming circulating immune complexes.
Delayed food reactions may affect any organ or tissue in the body. Common conditions where food sensitivity may play a significant role include abdominal bloating and fluid retention, inflammatory bowel disease, irritable bowel syndrome, migraine, depression, mood swings, asthma, skin conditions, and behavioral problems in children.
Clinical Applications for IgG Food Sensitivity Testing
It has been found that an increased IgG antibody level to foods, especially to egg white, orange, and a mixture of wheat and rice, is a positive predictor of increased IgE antibodies to inhalant allergens such as dust mite and cat and dog hair. Early testing for IgG food sensitivity in children may, therefore, identify children with an increased risk of developing future allergic disease. An aggravation of neurological symptoms has been reported in autistic patients after the consumption of milk and wheat. On testing, it was found that the level of IgG antibodies for casein and other milk proteins was significantly higher in this group than those of the control group. Following a period of eight weeks on an elimination diet, there was a marked improvement in behavioral symptoms. In another study, patients with rheumatoid arthritis placed on a gluten-free diet showed a decrease in IgG serum levels, which correlated with an improvement in symptoms of the disease in 40% of subjects, compared to a 4% improvement in the control group, over a one year period. The IgG immunoglobulin has four subclasses: IgG-1, IgG-2, IgG-3, and IgG-4. Significant reactions are mediated by all four, so it is important to screen for all of them. Testing for IgG-mediated food reactions can be utilized in conjunction with case history and other relevant test results, such as intestinal permeability, as an efficient and reliable method for diagnosing patients with adverse reactions to food/s. Sensitivity is identified by screening blood samples for IgG antibodies to a panel of foods. The most common reactions occur with cow’s milk, eggs, beans, nuts, and cereals.
Case studies done by Cambridge Nutritional Sciences, Eden Research Park, UK, on some of the symptoms and clinical conditions are briefed below:
Going to family gatherings becomes a difficult experience, as it becomes excruciatingly painful at times of bloating and constipation. Irritable bowel syndrome sometimes causes you to miss work. People keep taking antispasmodics, which do not help in the long run. The only remedy is to find out what the “poison food” is for you. On receipt of the food intolerance tests report, with recommendation to avoid some of the foods that are taken in everyday life, the problem gets solved, and happy face looks forward to parties, besides being punctual at work.
In one subject with persistent headaches nearly every day for the last four years, painkillers never helped. After knowing the culprit, and avoiding wheat, cow’s milk, and soya milk, which was a little difficult initially, though, it worked out well to get rid of the persistent headache.
A subject, a second-year business studies undergraduate, was becoming increasingly concerned about his complete lack of energy; he felt constantly drained, was always tired, even after a good night’s sleep, and was finding it virtually impossible to stay motivated at university. He did an array of different tests, including biochemistry, immunology, and hematology, but each test came back negative or normal. When his food intolerance test was conducted, it was found that he was intolerant to a wide range of foods, and many came out with a very strong reaction. They included cola nut, soya bean, barley, corn, rye, maize, yeast, wheat, pineapple, and grape. It was difficult for him to avoid such a list of foods, but had no choice; however, he felt energetic afterwards with some additional food supplements.
Another subject, a mother of three grown-up children, had suffered for 12 years from fortnightly migraines, unsightly spots on her neck and stomach, blisters on palate, trapped wind, and aching joints. “I was in a vicious circle of feeling unwell. Just as one symptom disappeared, another began,” she said. Having a physically demanding job as a farm worker made life doubly difficult. “Working in a hot greenhouse and bending down to pick strawberries was not pleasant when I was feeling so unwell.” Her mystery illness also prevented her from having a social life outside her immediate family.
“It was awful. I never liked to book things up in advance, in case I would let people down by getting one of my migraines, which would typically last three to four days and come every couple of weeks,” she continued. “I’d visit the doctor every six months, but although I was given pain management, nothing was done to get rid of the source of the migraines.”
A food intolerance test showed that she was reacting to soya bean, wheat, barley, corn, rye, cow’s milk, egg white and yolk, cola nut, pineapple, grapefruit, almond, and cashew nut. Desperate to feel normal again, she immediately avoided these foods and was better within a week. “I feel like a different person. I feel more alive, with so much energy, and I have started to enjoy life again, meeting up with friends and going swimming twice every week,” she said.
ME: Chronic fatigue syndrome, a medical condition where neurological and immune systems get affected and long-term fatigue and other persistent symptoms makes a person completely inactive, is also referred as Myalgic Encephalomyelitis (ME). Knowing the food that has IgG-mediated reaction (food intolerance), and avoiding that food contributes heavily during the treatment of ME.
Know your poison now.
 Medicosnext
Medicosnext




